Stem cell study sheds light on Klinefelter syndrome
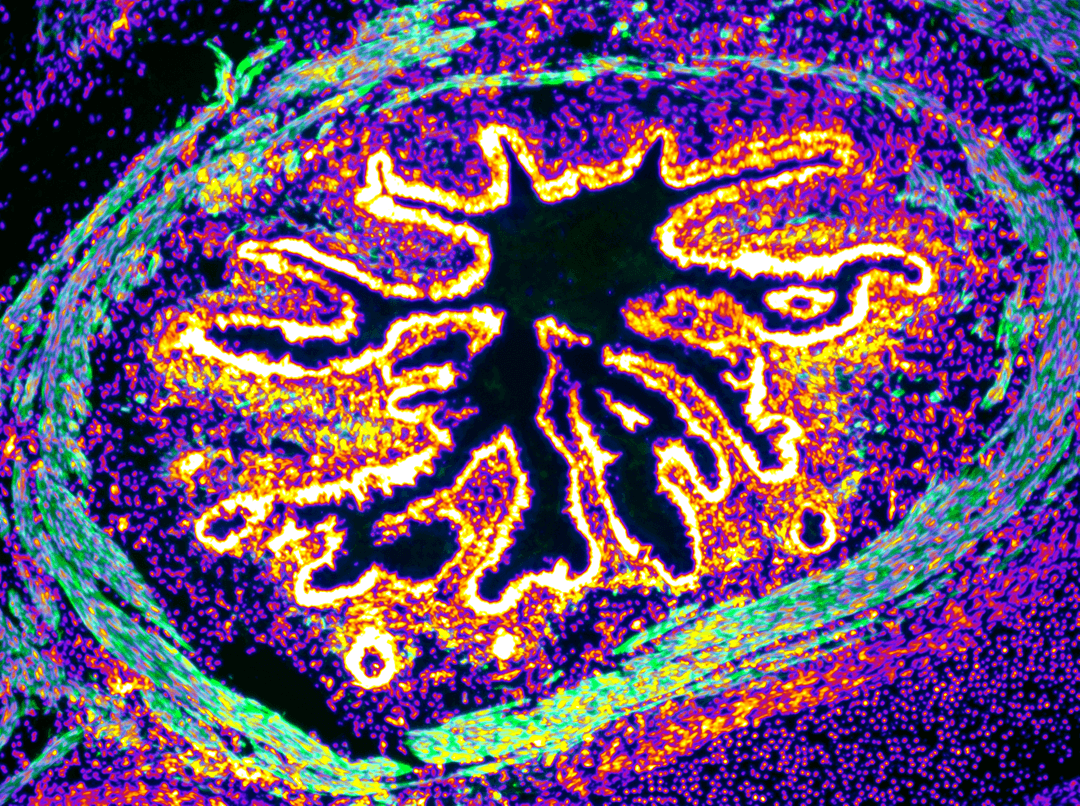
The teratoma is an embryonal tumor developing from pluripotent stem cells. In the laboratory, KAUST scientists use the Teratoma formation assay to prove that the patient-derived iPSCs are truly pluripotent. Photo: KAUST
In a research partnership between King Abdullah University of Science and Technology (KAUST), King Abdulaziz University, Jeddah (KAU) and King Abdulaziz University Hospital, Jeddah (KAUH), scientists have conducted a first-of-its-kind study in the Kingdom that compares stem cells derived from a unique cohort of Saudi Klinefelter patients with a group of North American and European descent.
Klinefelter is a chromosomal disease characterized by an extra chromosome X in the cells of males. Frequent clinical features of the syndrome are infertility, intellectual disability, metabolic syndrome and type 2 diabetes among others, and one out of every six hundred Saudi males are affected. However, the MENA population is largely underrepresented when it comes to studying the impact of the genomic background on disease susceptibility and prognosis. The majority of studies involving the use of iPSCs have been performed using North American and European patients.
The KAUST-KAU-HAUH study addresses this gap using a "patient-derived induced pluripotent stem cells" (iPSC)-based disease modeling study aimed at understanding the molecular basis of Klinefelter syndrome. By using skin, blood, hair or urine-derived cell samples with the iPSC approach, it is possible to bring the patient’s cells back to the embryonic state in which they developed, and use them to model the onset and progression of diseases “in a dish.”
“The Kingdom is benefitting from the world-class collaboration between our three leading research entities,” said Vice President for Research Pierre Magistretti, Distinguished Professor and director of the KAUST Smart-Health Initiative. “The iPSC technology is revolutionizing the study of the molecular mechanisms of diseases as it provides a way to work on human cells derived from patients.”
Magistretti added that the platform for iPSC that KAUST scientists have developed allow for unique collaborations with clinical centers such as KAU KAUH and with the support of KAUST KAUST Smart-Health Initiative Initiative.
The results from this first joint Saudi study demonstrate the existence of a subset of genes residing on the X chromosome, whose dysregulation specifically characterizes Klinefelter syndrome, regardless of the geographical area of origin, ethnicity and genetic makeup.
“This Saudi iPSC cohort will serve as an ideal cellular platform to explore further work into chromosomal diseases,” said Antonio Adamo, assistant professor and principal investigator in the Stem Cell and Diseases Laboratory at KAUST. “For example, it would be particularly interesting modeling neurodevelopment and anatomical changes affecting grey and white matters, features typically observed in Klinefelter Syndrome.”
This cellular platform will be used to generate the so-called “mini-brains,” three-dimensional cultures of patient-derived cells resembling the human brain that can be used to study the molecular mechanisms underlying the neurodevelopmental features of the disease. The findings yield an in vitro model suitable for the development of personalized medicine applications.

